The Health Ministry’s move to partner with the private sector comes amidst a dwindling number of available ICU and normal beds in public Covid-19 hospitals.
This shortage comes as active cases, deaths and Covid-19 patients with severe conditions rise dramatically.
This is according to a Jan 14 document prepared by the ministry’s Crisis Preparedness and Response Centre (CPRC) and presented to the top management of several private hospitals on that day. Malaysiakini has sighted the document.
The ministry classifies Covid-19 cases into categories, the most severe being Category 4 (patients with pneumonia and requiring oxygen) and Category 5 (patients with critical illness and multi-organ failure).
In the first week of December 2020, Category 4 and 5 patients made up almost one in 50 Covid-19 patients (1.93 percent).
Less than a month later on Jan 4, 2021, these patients now made up about one in 10 Covid-19 patients (9 percent).
Covid-19 related deaths have also seen a rapid increase in recent months. The first nine months of 2020 recorded less than 100 deaths cumulatively.
Then in October 2020 alone, 113 people died from the virus. November and December saw 111 deaths each month.

Covid-19 deaths in the first 15 days of 2021 now total 115. The ministry projects 280 people will die from the virus in January alone unless there are interventions.
ICU beds low in 10 areas
The worsening pandemic has caused Covid-19 hospitals in 10 states and territories to run low on ICU beds.
CPRC data dated Jan 14 showed that the situation is most dire in Selangor.
Of the 60 ICU beds in Hospital Sungai Buloh, 55 were filled as of Jan 14. This amounts to a 92 percent utilisation rate.
Malacca is a close second with a 90 percent utilisation rate. Forty-seven of the 52 ICU beds in Hospital Melaka are utilised.
Even with five Covid-19 hospitals, Perak ranks third in terms of ICU bed utilisation rate at 86 percent. Sixty of its 70 ICU beds are filled.
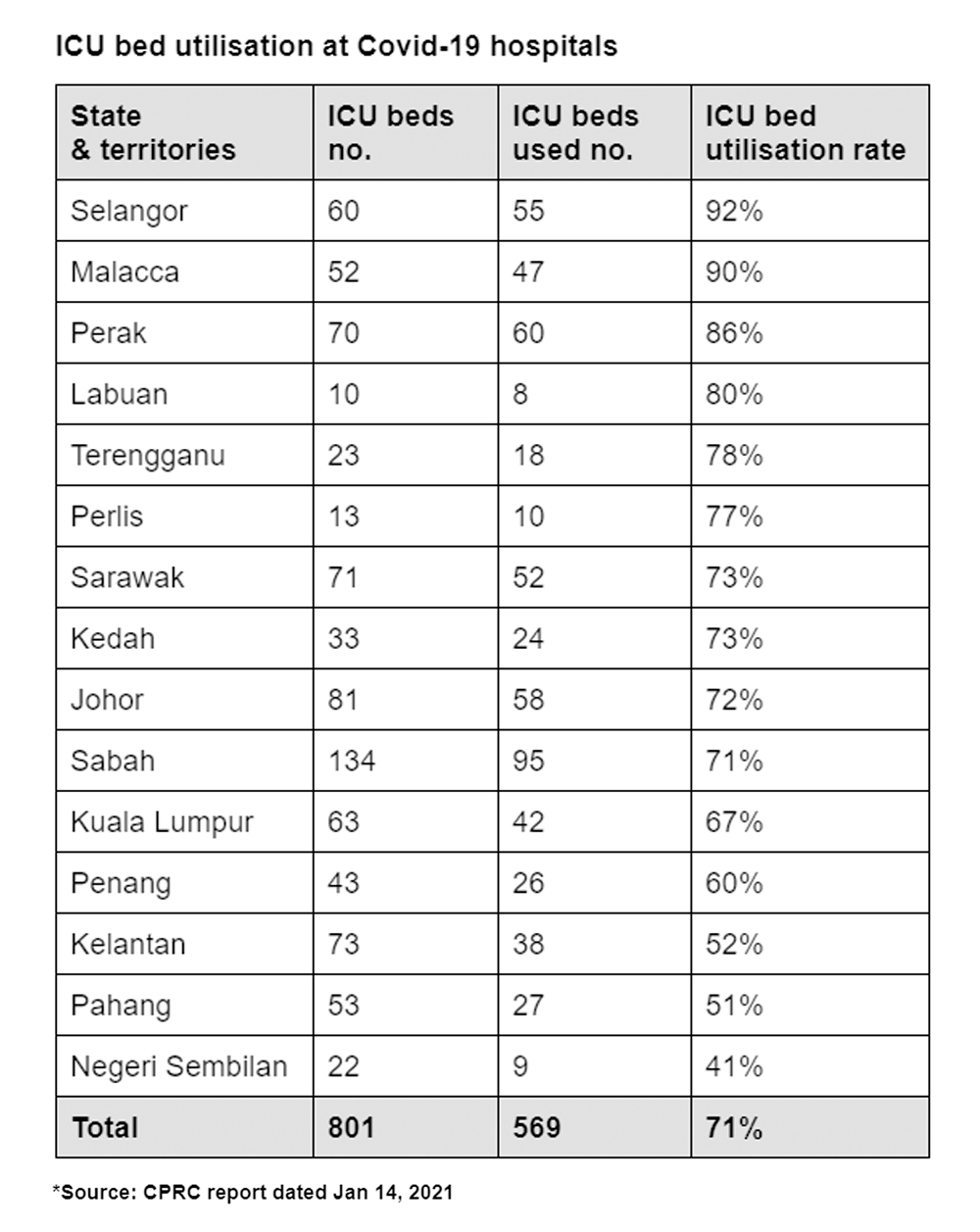
The other seven areas where Covid-19 hospitals had more than 70 percent of their ICU beds filled are Labuan, Terengganu, Perlis, Sarawak, Kedah, Johor and Sabah.
As of Jan 15, Malaysia had 204 Covid-19 patients in ICUs where 87 of them were intubated and on ventilator support. This figure does not include “suspected” or “probable” Covid-19 patients who are also placed in separate ICU.
This is the highest number of ICU patients the country has seen since the pandemic began.
Other critical patients affected
According to the CPRC, the ICU bed shortage at Covid-19 hospitals has had a knock-on effect on other hospitals and patients with other critical conditions.
Public hospitals that typically do not treat Covid-19 (non-Covid hospitals) are now unable to transfer their ICU patients who have Covid-19 to designated Covid-19 hospitals.
This means there are now less ICU beds for patients with other critical conditions at non-Covid hospitals.
The situation has further exposed healthcare workers at non-Covid hospitals to the virus.
The non-Covid hospitals most affected by this situation are mostly in the Klang Valley.

One example is Selangor’s Hospital Serdang, which has a total of 19 ICU patients who are confirmed or suspected of Covid-19.
Normal beds also running low
Aside from ICU beds, public Covid-19 hospitals in six states are also running low on normal beds.
States with more than 70 percent of their normal beds filled are Kedah, Penang, Johor, Selangor, Perlis and Negeri Sembilan.
The three Covid-19 hospitals in Kedah are almost at full capacity with 204 of their 213 available beds filled. This constitutes a 96 percent utilisation rate.
In second place is Penang, where 197 of the 224 beds in Hospital Pulau Pinang and Hospital Kepala Batas are filled (88 percent).
Johor ranks third with 590 of the 708 beds in its three Covid-19 hospitals filled (83 percent).
Malaysiakini understands that the CPRC briefed three of the country's biggest private healthcare providers - IHH Healthcare Bhd, Ramsay Sime Darby Healthcare and KPJ Healthcare Bhd - about these numbers last Thursday.
How to integrate private sector
At the time of the briefing, the ministry had close to 2,000 personnel who were out of action either due to Covid-19 infections or in quarantine after being identified as close contacts.

To solve the facility and human resource shortage, the CPRC proposed a “conceptual model” that integrates the private sector into the government’s Covid-19 response mechanism.
The plan ropes in private hospitals, private clinics, e-hailing service providers and private ambulance providers.
It proposes that private hospitals that are designated as Covid-19 facilities admit Covid-19 patients including those requiring ICU care.
The plan requires these hospitals to continue treating Covid-19 patients for as long as they need care. This could mean they may not be allowed to refer or transfer patients to public Covid-19 hospitals.
Other private hospitals will be required to take on non-Covid patients from public hospitals, including emergency and semi-emergency cases.
Malaysiakini previously reported that the ministry has also begun negotiations with the Association of Private Hospitals Malaysia (APHM).
Among the proposals was for private hospitals to allocate 10 percent of their normal and ICU beds for Covid-19 patients.
Some of the payment options discussed were to compel insurance companies to cover patients with medical cards or have Covid-19 patients foot their own bills if they are treated in private hospitals.
Should the pandemic worsen and public hospitals be compelled to refer patients to private hospitals, the Finance Ministry could be roped in to design a mechanism to help those without the means to pay for their private healthcare bills. - Mkini




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.