Recently, I wrote about how to avoid a Covid-19 disaster in Malaysia. This crisis has washed over us and the toll in deaths and loss of livelihood has been and continues to be significant.
I am now writing about the impending, massive fifth wave. This wave may be so big as to make the current one look pale in contrast. In a sense, we have, in the fourth wave, experienced what Italy did last year. Now the fear is that we may experience what India, Peru and some other countries in South America are experiencing.
Some of our leaders seem to live in denial of the reality; one even saying that the pandemic in Malaysia is under control. Others have set a value of '4000 cases' as a benchmark to use, but in the face of high positivity and limited testing, this is fraught with problems. A good look at the data and trends suggest that the worst may be yet to come.
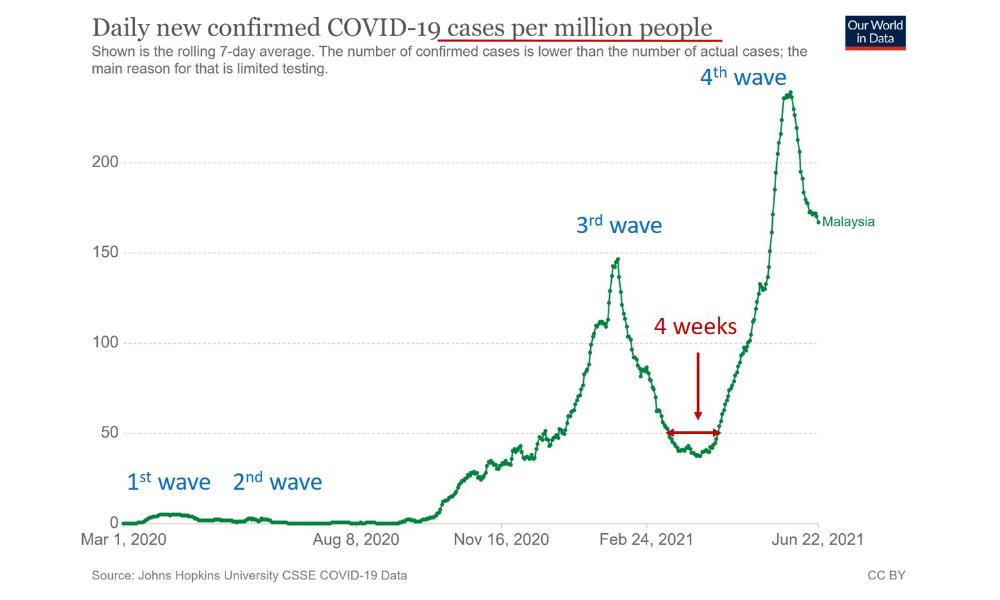
When will a fifth wave potentially hit us? The graph below shows the growth of the Covid-19 outbreak in Malaysia in relation to the population (seven-day averaged data to offer a more accurate picture).
You can see that the fourth wave came very quickly after the third wave; as fast as four weeks after the third wave. Some may argue that the fourth wave was due to considerable movement of individuals related to the puasa month and Hari Raya period; that this encouraged the spread.
But the real issue is that, even now, we fail to understand that there is no safe number to meet. All social interactions at work, education, religious or otherwise are easily exploited by this virus.
The current high baseline community infections, predominantly unlinked, makes another surge very likely.
Why will a fifth wave come?
The fifth wave will come for a number of reasons. Firstly, we cannot continue lockdowns indefinitely; the suffering of the poor and middle class is enormous. It has been estimated that an additional two to three million Malaysians have been pushed below the poverty line during the Covid-19 crisis thus far. The Small and Medium Enterprises (SME) Association of Malaysia is quoted as saying that approximately 100,000 companies have ceased operations since the first MCO and an additional 50,000 may lose their businesses with any extended lockdown.
So we will have to reopen the economy or face worsening poverty, malnutrition of children, rising suicide rates, etc. It should be noted that we have provided inadequate support for the poorer segments of the population and those struggling in terms of financial and mask assistance.
Secondly, we have yet to make significant changes to our work, business and education environments to reduce Covid-19 spread. We have continued to focus on surface decontamination instead of the more important ventilation to reduce airborne transmission. The lack of a national directive to do this hampers local initiatives.
Thirdly, our social responsibility remains limited. This applies to the leaders as much as to the people. Blaming the people without stern action against errant leaders and the rich does not promote collective community social responsibility in addressing this pandemic.
Finally, and perhaps a critical reason, is the Delta variant. Dr Mike Ryan, executive director of the World Health Organisation (WHO) said, during a news conference on June 21, that the Delta variant has the potential “to be more lethal because it’s more efficient in the way it transmits between humans and it will eventually find those vulnerable individuals who will become severely ill, have to be hospitalised and potentially die”.
Data is just coming in, but the Delta variant appears to be more contagious and vaccines to be less effective against it. The limited genome testing done locally shows that the Delta variant is present in many states but we need more data to track its spread. Data from some nations show that the Delta variant rapidly becomes the dominant infective strain and reverses some of the progress that has already been made.
Won’t our vaccination programme save us?
Vaccinations are a key component to bringing the Covid-19 pandemic under control. While we have had a slow start to vaccination, we are now vaccinating at an accelerated pace. However, the impact of our vaccination may not ‘kick in’ fast enough. Many hope our vaccination will save us, but we still require about three months to get 50 percent of our population vaccinated with two doses. There is also an unacceptable disparity in vaccination supply between states which may leave some regions less well protected.
Note also that many vulnerable people have yet to be vaccinated. As of June 20, we have 937,078 registered senior citizens who are still waiting for appointments. Only 19,000 (6.8 percent) out of 280,000 adults with disabilities who registered have received the first dose. We have no idea of vaccination rates among adults with comorbidities like diabetes, hypertension and heart disease; they comprise ~30 percent of the adult population with many under 60 years of age. Note that there are many more of these three vulnerable groups who are either not able to register or are hesitant. They will be the ones hard hit by a fifth wave.
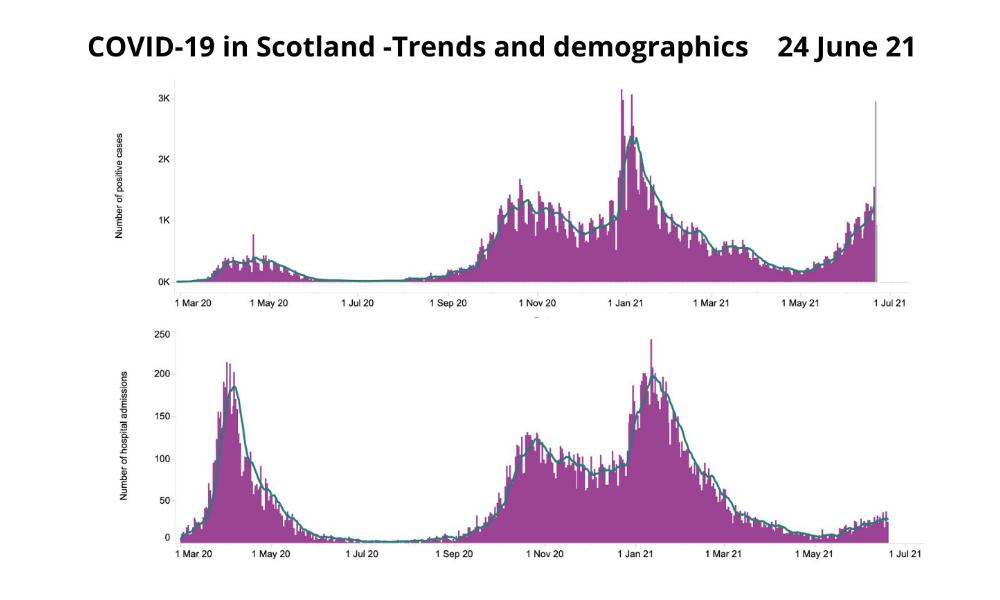
Note that even nations with high vaccination rates are beginning to see a rise in cases and hospitalisations due to the Delta variant. Current data from Scotland (see graph below) from Dr Gabriel Scally, former regional director of Public Health England and a member of Independent Sage, shows that despite 48 percent of the population fully vaccinated, the Delta variant has caused a rise in cases and hospital admissions. While the majority who get infected are not yet vaccinated (showing good vaccine benefit), some vaccinated individuals also do get infected.
So vaccination will help but they need to reach a large segment of the population before outbreaks can be reduced.
Why will a fifth wave be more severe?
If we have a fifth wave very soon after the fourth we may not do as well. Our intensive care services (ICUs) are overstretched and still struggling with Covid-19 cases with some having adults who have been dependent on ventilators for a long time. The health system has chronic fatigue, not just in hospitals but also in the public health sector and vaccination centres. If we have a fresh surge due to the Delta variant, the system has little reserve to cope.
How can we work together to minimise the fifth wave?
Covid-19 has been dubbed the “unforgiving virus”. Any failure on our part will be exploited to infect us or spread the disease. The key is to avoid getting infected. This requires a shared responsibility that is built on trust and discipline (routines) between everyone – especially if you are working or studying outside the home; what we like to call ‘trust bubbles’. As always, remember to improve the quality and fit of your mask.

We need to follow the data and science when working to minimise Covid-19. Sharing all our Covid-19 data will help the public make better-informed decisions. Some suggestions to minimise the fifth wave include:
1. The only good vaccine is the one in the arm of a person
We need to administer all our vaccine supply to the public as quickly as possible. There should not be any vaccines left in the storehouses and all PPVs (Pusat Pemberian Vaksin) in the country should be supplied according to their population numbers. The second dose should be given at the minimum duration possible (shortest data-based interval possible). Ramping up daily vaccinations to the highest possible (based on supply) is critical; 300-400,000 doses a day are necessary.
2. Speed up the vaccination of the vulnerable
In the next four weeks, we should focus on completing the vaccination for all registered senior citizens, adults with disabilities and adults with comorbidities. In addition, we should proactively search for these vulnerable groups who have not been able to register or are hesitant and offer them vaccination appointments. Parents of children with disabilities should also be prioritised for vaccination to protect their vulnerable children; as should all those involved in child care and pre-school services.
3. Test, test, test
We need to test widely and not allow 60-80 percent of cases to be unlinked. We have to test asymptomatic contacts of identified cases and not just those who present with signs of an infection. Using reliable antigen rapid test kits (RTK-Ag) for community testing and polymerase chain reaction (PCR) tests for admissions will be the best utilisation of resources and offer quicker results. A total of 200-300,000 tests a day should be our minimum.
We need effective contact tracing and isolation mechanisms. Digital contact tracing and alerts must occur in real-time for this to happen.
If possible, we should offer cheap, weekly RTK-Ag tests for all those going to work in any sector to limit clusters from developing. We need to work towards developing and maintaining 'work safety bubbles'.
4. Home safety bubbles, even for the vaccinated

For all of us, we need to limit all unnecessary contact with others to maintain a home safety bubble. Don’t visit your extended family or grandparents and don’t stop to talk to your neighbours when doing your morning walk – speak to them via a video call. Stop all family and religious gatherings, even in small groups – there is no safe number.
Those who are vaccinated should continue to maintain the normal Covid-19 prevention measures like everyone else. It is important not to relax our vigilance at this time.
We are concerned this pandemic has damaged our children, especially with the loss of schooling. But in the current crisis, keeping children at home and continuing their education there is the right move. Many children (40 percent) have no digital devices or Internet connections. We need to work together as a community to ensure they are supported.
5. National ventilation mandate and streamline SOPs
We now know that the Covid-19 virus is primarily spread by airborne mechanisms, especially indoors. Keeping a 1-2 metre distance in a room is of little value unless you improve the ventilation. We need a national initiative to improve ventilation in all buildings and maximise the intake of outdoor air. This means encouraging fresh air to come in all the time and stopping recirculation of air by air-conditioning units.
The current standard operating policies (SOPs) are not all science-based. Many are burdensome to the public. Even temperature scanning has little value and should be stopped. Time to revise all the SOPs, remove many and streamline them to include only the meaningful ones. This will improve compliance and effectiveness.
We must not be complacent about the threat of a fifth wave in Malaysia, especially due to the Delta variant. Our pandemic is barely under any control despite four weeks of a lockdown. We need to support each other and see the nation through these next few difficult months.- Mkini
DR AMAR-SINGH HSS is a consultant paediatrician.
The views expressed here are those of the author/contributor and do not necessarily represent the views of MMKtT.




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.