COVID-19 | As Malaysia enters its fourth week of movement control order (MCO) lockdowns, the number of active Covid-19 cases continues to climb and one contributing factor is the testing backlog.
Backlog slows down public health response's ability to isolate cases and stem the spread. This can end up straining the healthcare system and even lead to a loss of lives.
In late January - when new cases breached the 5,000-mark thrice despite lockdown measures - the Health Ministry admitted that backlogs dated as far back as 2020.
This article aims to explain the cause of the backlogs and propose possible solutions.
So how are Covid-19 cases reported?
When a Covid-19 positive case is detected, information about the case needs to be communicated to the:
- Public Health Laboratory Information System (Simka)
- Institute of Medical Research (IMR)
- District health office
Laboratories must log both positive and negative RT-PCR results into Simka. Overseen by the National Public Health Laboratory (MKAK), it is a centralised data portal for all infectious diseases.
One laboratory told Malaysiakini that it is required to inform IMR as well.
Laboratories next need to inform doctors of the results.
Doctors must then relay information on positive cases to the local district health office so that actions such as contact tracing can be performed.
What causes the delay?
Health director-general Dr Noor Hisham Abdullah explained in an online media briefing on Friday (Jan 5) that backlog occurs when laboratories struggle to process swabs quickly.
This can happen when laboratories are overwhelmed by the number of samples they receive.
The backlog is also caused by delays or errors when uploading data into Simka.
“The delays usually happen at private laboratories who do not key in negative test results. But now, we are also seeing delays in reporting positive test results,” said the top official.

There are 68 RT-PCR laboratories nationwide - 23 of which are privately owned while the rest are run by public hospitals (21), MKAK (7), the Armed Forces (3), universities (13) as well as the Science, Technology and Innovation Ministry (1).
Noor Hisham said data integration between Simka and these laboratories was another challenge.
Laboratories typically have their own Laboratory Information Systems. This means they need to input data twice - once into their own database and a second time into Simka.
Why do private labs face delays?
However, some private laboratories have managed to cope by employing dedicated data-entry teams and investing in technological solutions.

Pantai Premier Pathology Sdn Bhd CEO Mohd Hareeff Muhammed told Malaysiakini that he has a specific team that focuses on keying information into Simka as quickly as possible.
This, he said, has enabled them to meet the ministry’s standards.
“Pantai Premier Pathology has a dedicated team that performs daily uploads of Covid-19 RT-PCR test results via Simka’s bulk upload function,” he said in an email interview.
Pantai Premier Pathology laboratories process Covid-19 samples from IHH-owned private hospitals, private GP clinics, government hospitals and corporate clients.

Meanwhile, BP Healthcare deputy president Joevy Beh shared that his staff initially struggled to manually record Covid-19 case data. The entire process has since gone digital.
BP now gets patients to submit all necessary information from the start when they book a test on its website. This data is then contained in a barcode to be used for the swab, laboratory test and data reporting procedures. Patients are notified of their results via an app.
Unlike most clinics and laboratories, BP can perform RT-PCR swabs and laboratory tests from the same facility. This helps cut down transportation issues and turnaround time.
This also creates a data hub for Simka data entry and for in-house doctors to inform district health offices about positive cases. Beh said BP emails test results to IMR as well.

For industry peers struggling with Simka reporting, he observed that delays often stemmed from incomplete patient information.
This means laboratories need to go back to clinics for more data. Clinics, meanwhile, might not be able to field every request due to workload and patient privacy issues.
“The laboratories will have the relay (what they need) to the private healthcare facility.
“Then the private healthcare facility will have to call the patients. It is quite a tough job. Imagine you are a clinic and you only hire three or four people but you are managing a few hundred patients,” Beh said.
Why do private GPs face delays?
Private GPs, meanwhile, accused laboratories of being the ones causing delays.
Dr Boo Cheng Hau, who conducts Covid-19 tests from his clinic in Johor, said he has waited up to four days for test results from laboratories.
“In my case, I had to chase and track down (my patients’) results when they should have informed the referring doctor,” he said when contacted.
Late test results cause a ripple effect on the entire Covid-19 response mechanism.
GPs will be slow in informing the district health office about positive cases. This in turn causes contact tracing delays, which risks exacerbating the spread of Covid-19.
Aside from slowing down public health response, this also delays data collection. Data from district health offices is collected by state health departments and reported to the Health Ministry, which compiles them to present national daily case numbers to the public every evening
Boo shared that delays also occur when laboratories do not provide all the required data points to doctors. This means doctors will need to contact laboratories for more information.

Moreover, district health offices require doctors to log a long list of patient data when reporting positive cases via the ministry’s e-notification portal or other avenues.
This includes a patient’s occupation, work address, symptoms, co-morbidities and Covid-19 test cycle threshold (CT) value.
This e-notification reporting process is further hampered if clinics face challenges in contacting patients for information district health offices need.
For Selangor GP Dr Gurnam Singh Sarjit Singh, language barriers can be an issue.
“(We face) language barrier problems if the patients are foreigners (and we) we ask them their home or work address.
“And some of them refuse to answer calls,” he said when contacted.
Nevertheless, Gurnam said his Ampang clinic would typically go ahead to notify the district health office with whatever information he had about a case.
Unlike hospitals or large-scale private laboratories, many clinics are smaller set-ups with only a handful of staff handling both clinical and administrative work.
According to Kuala Lumpur-based GP Dr Shanmuganathan Ganeson, e-notification reporting delays can happen when patient numbers are high.
“Clinics only have a few staff members. If there are too many positive cases, then the capacity of clinics to cope is overwhelmed.
“Clinics may also be busy with other patients, other reports, ill patients requiring complicated care or other pressing administrative tasks. All these can occur without warning,” he explained.
Shanmuganathan said he knew of one clinic that had to employ additional staff just to enter Covid-19 patient data into the e-notification system.
Nevertheless, the Federation of Private Medical Practitioners’ Associations Malaysia (FPMPAM) honorary secretary said clinics were trying their best and maintained that delays were rare.
Like private laboratories and clinics, Shanmuganathan wondered if district health offices were also struggling to cope and contributing to the backlog.
How can delays be resolved?
Noor Hisham has been talking about case reporting delays since late last year, indicating that this has been a perennial problem.
He now wants laboratories to “step up” by employing more staff, redesigning internal processes and improving data integration.

According to MKAK director Dr Hani Mat Hussin, Simka has been upgraded to facilitate bulk uploads to make it easier for data input.
“So previously, they (private laboratories) will perform full data entry for their own Laboratory Information System and also our Simka.
“But at present, they only need to input data into (their) system and transfer or bulk upload it into Simka. So maybe that will reduce their burden in keying in data,” she told a media briefing on Friday.
However, even with the upgrades, the process of uploading data is still laborious, prompting Selangor government start-up SELangkah to design a computer programme that automates data input into Simka.
SELangkah team member Dr Helmi Zakariah told Malaysiakini that his colleague Mellwvn Chew created the Aimenah bot back in December 2020 to assist GPs who were struggling to cope with data entry.
This is especially for GPs who are conducting mass screenings using antigen-based rapid test kits (RTK-Ag), which can be processed at clinics. Not only do they need to upload results into their own LIS and Simka, but they also need to inform district health offices about positive cases.
Helmi explained that patients will first register for an RTK-Ag test on the SELangkah app and fill in their information. They will be given a digital barcode for their test. After the test, the GP will report the result to their own LIS. Aimenah will then immediately transfer the data into Simka.
“This removes the redundancy of double-entry,” he said.
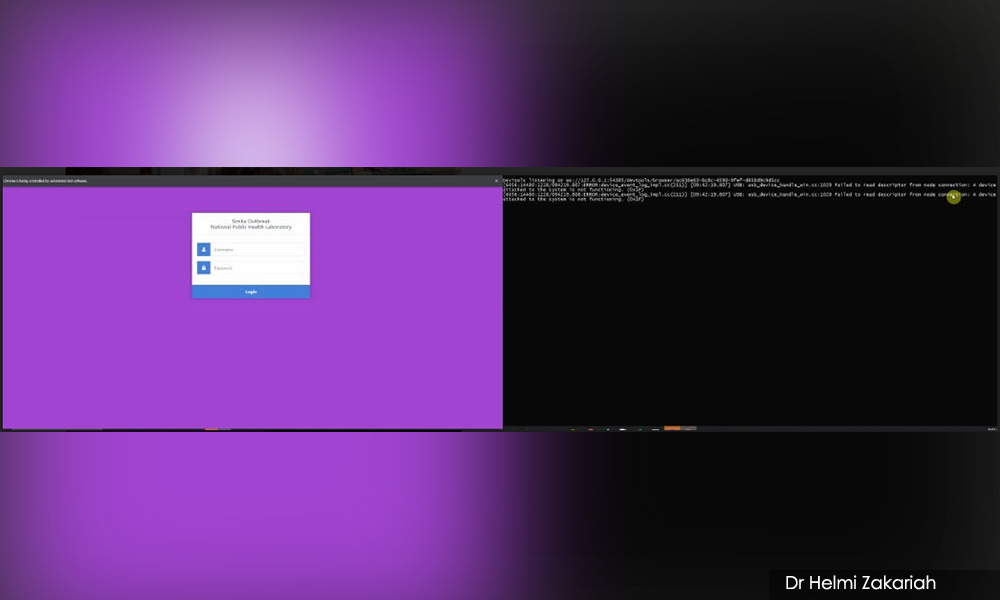
Helmi said that Python-based Aimenah is capable of automatically entering 800 datasets into Simka in a day. Seventeen GPs are currently utilising the bot.
“These are the number of GPs who reached out to us at SELangkah to ask for help once they knew we had this bot solution.
“These are the same GPs who are helping to extend the screening capabilities of the entire country. Hats off to them,” he said.

Meanwhile, GPs like Boo have decided to employ more low-tech workarounds.
Instead of using the e-notification portal, he finds it more efficient to send information about positive cases through WhatsApp. Patient data is typically organised according to a template and sent as a text message to the local district health office’s WhatsApp hotline.
GPs can also call or email their local district health offices instead.
To improve the reporting process, Boo proposed that GPs be allowed to directly input data on positive cases rather than having to go through district health offices.
“For better service, district health offices should be given the power to recruit GPs for assistance in assessing patients and reporting them to a centralised data pool managed by the office, the state health department and the ministry,” he said.

Selangor Menteri Besar Amiruddin Shari previously threatened to fine private clinics and private hospitals an undisclosed amount for delays in Simka data entry.
This was after the state saw a dramatic spike of cases due to a 10-day backlog from mass screenings.
However, he was severely criticised for his harsh attempt at solving the problem.
The Malaysian Medical Association condemned the “accusation” and said private healthcare facilities were not to blame. The Association of Private Hospitals Malaysia concurred and called for empathy for overwhelmed private laboratories.
Private laboratories are already struggling to cope despite collectively testing at 31 percent, far under what they are capable of.
However, the ministry now has ambitions to raise Malaysia’s total maximum RT-PCR testing capacity from 76,805 to 200,000 tests a day.
Queries about Aimenah can be made by contacting SELangkah by email at izlan@aime.life or via their WhatsApp hotline available on their website. - Mkini




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.